Today, it’s estimated that at least 154,000 people in the U.S. have Stage IV, or metastatic, breast cancer. Although metastatic breast cancer currently cannot be cured, it can still be treated – focusing on living a longer, healthier life with breast cancer. In this episode, Carol Smith shares her story of living with MBC.
About Carol
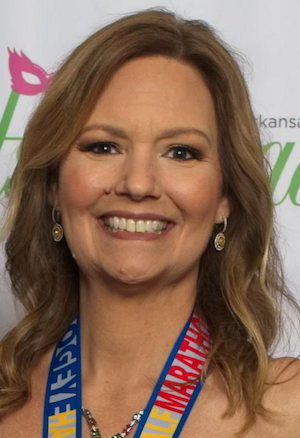
Carol Smith is living with metastatic breast cancer. Carol was diagnosed with stage one hormone receptor-positive, HER2 negative breast cancer in 2013.
After back pain in 2015 and an MRI, she found out that the breast cancer had moved into her spine and was then diagnosed with stage four or metastatic breast cancer.
Carol focuses on living a healthy livestype and enjoys running, tennis, and previously completed a half a marathon every month.
Transcript
Adam: [00:00] No matter how long ago someone was diagnosed with metastatic breast cancer and no matter the struggles someone faces today, there are likely other people who share the same challenges. Today it’s estimated that at least one hundred and fifty-four thousand people in the US have stage four or metastatic breast cancer. Although metastatic breast cancer currently cannot be cured, it can be treated focusing on living a longer, healthier life with breast cancer. Today I have the pleasure and honor of talking with Carol Smith. Carol, welcome to the show.
Carol: [00:30] Thanks Adam, glad to be here.
Adam: [00:31] Well, give us a little bit about your story. Tell us about you.
Carol: [00:34] I was diagnosed with stage one hormone receptor-positive, HER2 negative breast cancer in 2013. That’s a pretty common type of breast cancer and it was a small tumor in my breast, so to treat it, I had two surgeries to try to get all of the tumor out, four rounds of chemotherapy and then thirty rounds of radiation to try to get rid of all the cancer. I then went on taMoxifen after my treatment and then started living my life, continuing, try to go back to a normal life. I was eating right. I was running, I played tennis. I was in the best shape of my life doing about half a marathon every month.
Adam: [01:11] Wow.
Carol: [01:12] Yeah, and then in late 2015 I started having some back pain and it got worse and worse and we did an MRI and found out that the breast cancer had moved into my spine. This was not bone cancer, this is breast cancer that had moved into my spine, then was diagnosed with stage four or metastatic breast cancer. So I had surgery to shore that up on one of my vertebrae and radiation on a couple of other spots in addition to the first spot where the cancer was seen. Started on some drugs to try to keep the cancer at bay because this, as you said, is not curable, but it is treatable. So I started on a new drug at the time, which was called Ibrance and then a complimentary drug called Letrozole. I also started a bone-strengthening drug to make sure my bones were healthy, even though I had cancer in them. Not that long after that, I had some more cancer in my bones, so I switched up the Letrozole to another drug called Faslodex and I stayed on that combination for a total of about two years.
[02:04] So in February last year I found out that the cancer had moved to my liver as well, not fun to hear about, so I had to change drugs again and this time I moved to a drug called Capecitabine which is also called Xeloda. And that drug worked for a little over a year and then found out that I have more cancer in my liver, and so about a month ago I started on another set of drugs called Verzenio, and we’ll know actually probably later today if the drug is working. I had some blood tests actually this morning to see if that drug combination is holding back the cancer or if I may have to switch drugs again.
Adam: [02:41] Wow.
Carol: [02:43] Yeah, I know and I’ll be on some kind of medication for the rest of my life basically trying to keep the cancer from progressing as long as possible, but it’s very likely, to be real, that it will kill me in the next few years given the statistics.
Adam: [02:55] Wow, that is quite the journey and I imagine a lot to overcome. So just walk us through just a little bit more about it, just so we can understand a little bit more about what metastatic breast cancer is. So what does that actually mean? What is that?
Carol: [03:11] So to put it in the easiest terms of how I explain it to my mom and my elderly grandmothers is that it’s breast cancer cells that have left the breast and taken up residence in another part of the body and then grown.
Adam: [03:25] Okay.
Carol: [03:25] We don’t know why that happens. Why it happens for some people and not for others. It can happen a year after your initial treatment or twenty years after your initial treatment or anywhere in between and really thirty to 40% of the women and men who have stage one through three breast cancer, one, two or three breast cancer, will have it recur elsewhere in the body and become metastatic at some point in their lives.
Adam: [03:48] Okay. I see I see. Okay.
Carol: [03:49] Yeah.
Adam: [03:50] And so is there anything that you’d like people to know about metastatic breast cancer. Obviously, you’ve experienced it a much deeper level than most people, so what do you want us to know about that?
Carol: [04:03] So a couple things. One, it’s incurable. The average lifespan of someone who has metastatic breast cancer is about three years.
Adam: [04:11] Okay.
Carol: [04:12] I’m at three and a half so I’m kind of a little bit beyond that, but depending on your type of breast cancer cause there are a number of different subtypes, the treatment options will vary and they are really, really specific to your type of breast cancer, so you really need to make sure you understand that. And then I have a couple of things to think about for people who have been diagnosed with breast cancer and are worried about if it’s spread. There’s a couple of signs to look for, would that be helpful?
Adam: [04:38] Yeah, yeah, that’d be great.
Carol: [04:39] So sure, so the couple of things to think about are that if you’ve got things like sudden weight loss or muscle or bone pain that doesn’t go away or gets worse after a few weeks so it feels like it’s something other than something that happened with your working out or something else. If you’ve got shortness of breath or coughing or something that doesn’t get better with antibiotics or some other kind of treatments. If you’ve got shoulder pain on your right shoulder, actually that can indicate cancer in your liver or if you’re just feeling kind of off for more than a couple of weeks. If you’ve had breast cancer or even if you haven’t had breast cancer, go to your doctor and insist, I mean they may choose to not believe you so insist on an MRI or a CT scan of your torso or wherever the pain is to get it checked out.
Adam: [05:23] Yeah.
Carol: [05:23] You’d rather be safe than sorry. If it is cancer, you really want to get that taken care of as quickly as possible and start on whatever appropriate treatments are so you really have to be kind of vigilant even if you have had even just stage one breast cancer that looked like it had been totally treated and it was ten years ago.
Adam: [05:40] Right.
Carol: [05:40] If something’s not feeling right, you really need to get that checked out.
Adam: [05:43] Yeah, and that’s something that a lot of guests have talked about it. If something doesn’t seem right with your body, trust your instinct, you know yourself, go get it checked out. Be your own advocate, right, because a lot of times that’s not easy to do.
Carol: [05:57] Yeah, you really, really do have to be your own advocate. Breast cancer, especially metastatic breast cancer treatment is not an exact science. While there are a number of drugs that have specific treatments for specific types of cancer, the order in which you can do them or how you might incorporate something like radiation therapy in addition to drug therapy really kind of varies based on you as a person and also as well with palliative care. What kind of pain management or complementary therapies you need really are going to vary based on who you are and where your cancer is and how you’re feeling. And if you’re not comfortable doing that yourself, find a friend, find a relative to help you in those conversations with your doctor in your care chain.
Adam: [06:35] Yeah, that’s something we don’t think about it. We can have other people be our advocates that we could take them with you, right to a point they can be your advocate.
Carol: [06:40] Oh yeah, totally.
Adam: [06:40] So going back just a moment to the journey that you’ve been on you know you listed the medications and all that and it’s just astronomical, I’d imagine. And so how have you coped with that? How have you coped with a diagnosis and then all of the bumps along the road, but from then until now?
Carol: [07:02] Yeah, it’s been an interesting challenge, Adam. I mean when I was first diagnosed with metastatic breast cancer, I thought I was going to die immediately. I really did. I had no kind of basis for understanding. I don’t have any kind of genetic markers for breast cancer in my family even though I do have breast cancer in my family, so I had no frame of reference on this. I thought I was going to die.
Adam: [07:22] Right.
Carol: [07:22] And then after my cancer responded to the first treatments I was on, I realized I wasn’t going to die soon and I started getting used to what this new normal was like and then a little over a year ago the cancer progressed to my liver and frankly I was scared. Your liver has to be healthy to live. It’s got a very important function and so I was crushed, I was scared and I try to stay grounded and try to stay present in the moment and worry about tomorrow when the time comes, but to be very honest, it is incredibly frightening to have your doctor tell you that your cancer has progressed. It’s just really, really scary.
Adam: [08:00] Yeah.
Carol: [08:01] And I’ve chosen to just kind of mourn for a little bit or be scared for a little bit and then kind of suck it up and move on.
Adam: [08:07] Yeah, then you got to get up and keep moving, right, yeah.
Carol: [08:09] Yeah, definitely got it, got it.
Adam: [08:10] And speaking of that, keeping moving, you still won’t seem very active. So talk to me a little bit about how do you take care of yourself? What does that look like right now?
Carol: [08:20] Well for me I’m pretty lucky I’m not in any pain from breast cancer, so I’m very lucky in that regard and I try to be as active as I can. I want to be as strong as I can for as long as possible to withstand this lifetime of treatment that I’m on. I mean I’m going to be on some kind of treatment for the rest of my life and for me to be healthy and eligible for potential clinical trials or to even handle the next more toxic drug that comes down the way, I need to be as healthy as I can. So I run, I play tennis, I do crossfit kinds of things. I really do like running, that’s actually my favorite and I run fifty-two half marathons and seven marathons, all with cancer in my body.
Adam: [09:02] What?
Carol: [09:03] Yeah.
Adam: [09:03] That’s unbelievable, fifty-two half marathons and seven marathons, over what time period?
Carol: [09:12] So I started, my first half marathon was in January of 2013 so about eight months before I was diagnosed with breast cancer, but the cancer was still there.
Adam: [09:20] Of course, yeah.
Carol: [09:20] We just hadn’t found it.
Adam: [09:22] Yeah.
Carol: [09:23] In January 2013 was my first half marathon and I have done fifty-two half marathons.
Adam: [09:28] I feel like that’s like a Guinness Book of world records sort of thing right there you should apply for it. That’s unbelievable, that’s amazing.
Carol: [09:35] There are quite a few of us met athletes as I call them, who are women and I mostly know women who have done things like run the Boston marathon, run all seven major marathons and we don’t look sick because it’s not the cancer that causes us to look sick. It’s the drugs that we’re on.
Adam: [09:54] Yeah, right.
Carol: [09:54] That causes us to look sick. So if you were to meet me at a restaurant or whatever, you would never know that I had breast cancer by looking at me because I look like a normal, healthy middle-aged woman.
Adam: [10:05] Yeah, wow.
Carol: [10:07] I mean I also try to eat pretty cleanly. I try to eat a lot of salad. I drink a lot of water. I really like sleeping, so I try to get about seven or eight hours of sleep a night and mentally try not to worry too much about what might happen in the future. I have a really, really, really great therapist. I also try to get a massage every week, which helps me as well and I’ve had to work with some therapy with my family as well. I think that’s also important because my husband and my children have also had to deal with my diagnosis and so having us all kind of work through the fear and the issues and everything that comes up with somebody having cancer have really, really helped all of us deal with this diagnosis.
Adam: [10:43] Yeah.
Carol: [10:43] So it’s really just trying to take care of the best I can. Be as educated as I can about my own cancer and my own treatment options and stuff and just try to live every day the best I can.
Adam: [10:54] So a minute ago you mentioned that actually I think you said you refer to yourselves as Met athletes and so it sounds like you’ve got a bit of a community around you. Can you just talk a little bit about that? What has been the most helpful in creating that community of support around you?
Carol: [11:12] Well, I’m a big Facebook user, so for me going onto Facebook was where I kind of naturally started and there’s a number of groups on Facebook to join both. If anybody is on Facebook and looking for support groups, just type in metastatic breast cancer in the search area and you’ll find any number of Facebook groups that can be helpful for you if you want to, and I’m in a number of those that are both local in where I live in Ohio, or regional so that I can help when we talk about either doctors or treatments. There’s a bunch of national/international groups that are also super helpful on helping cope with side effects or learning about side effects or learning about new drug treatments or new clinical trials, all of that kind of stuff.
[12:01] And just kind of general support of somebody who else is there and has been there and can help you just kind of deal with the day to day living through this disease. And we all support each other and are there for each other when in the good days and bad days and you’re feeling crappy because your drugs or you’ve got really bad side effects and you just want to just vent to somebody. It’s a great way to do that. There’s other online support communities as well I’m just not as familiar with them, but there’s a ton of us online. And then we’re very fortunate where I live to have a local cancer support center and, for all types of cancers, and every month there’s a group session that’s facilitated by a social worker who is just in that group is just for metastatic breast cancer.
Adam: [12:44] Oh that’s great.
Carol: [12:45] And we get together every month and just kind of share what’s going on with our lives and again provide that in-person support and that’s really just a great way to provide additional face to face people who are living the same thing you are.
Adam: [12:58] Wow, that’s fantastic. So one last question, if you were able to give one piece of advice to a person listening to this podcast that is dealing with and living with metastatic breast cancer, what would that piece of advice be?
Carol: [13:14] That you have to be your own advocate. We touched on that a little bit before.
Adam: [13:17] Yeah.
Carol: [13:17] And I think that I cannot emphasize that enough. You have to work with your oncology team to get you the treatments and services that work for what you need. If you need financial support, you need to work with the social workers in your hospital or with your local common chapter to help you find additional financial support. If you need help managing your side effects, you’ve really got to talk to your doctor and your medical team about palliative care and supportive care to help you with whatever those side effects are. Whether it’s pain management or issues with your skin or issues with your gut or whatever they are you’ve got to insist upon getting that help. And if you’re in a hospital system that doesn’t have doctors that are specialists in breast cancer, if you’re in a smaller hospital, your oncologist may be somebody who deals with all kinds of cancers and unfortunately in that situation it’s even more incumbent upon you as the patient to work with your doctor to help that doctor understand what the new options are for you, including clinical trials because a lot of times there may be a clinical trial that is best for you and you’ve got to just find those yourselves because your oncologist doesn’t have time to do that for you.
Adam: [14:31] Right, right.
Carol: [14:31] Very few of them have time to do that so definitely try to find your voice either with yourself or with somebody else to help.
Adam: [14:38] I love that. Find your voice with yourself or with somebody else to help you to be your advocate. That’s really, really great. Well, Carol, this was great. I really appreciate you sharing your journey with us. It’s really impactful, very encouraging, and I really appreciate your time.
Carol: [14:54] Oh, you’re so welcome, Adam. Glad to help.
Sponsors
Thank you to Dragon Army for sponsoring this podcast.
